Introduction
Adhesive capsulitis, or frozen shoulder, causes pain and a clear loss of motion to the shoulder. It can arise from a traumatic episode, sometimes a fairly trivial trauma. It can also appear for no apparent reason. Patients in this instance will describe that they just woke up with it one day.
Anatomy
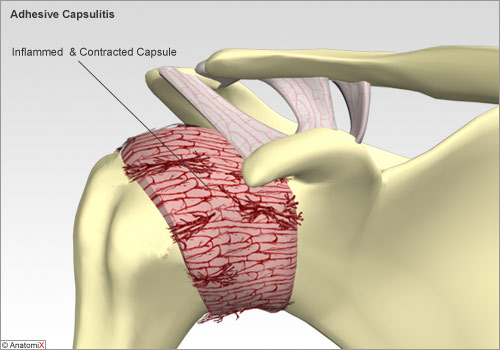
The problem in adhesive capsulitis is with the shoulder capsule. The capsule of the shoulder is a fairly complex structure that includes the static shoulder ligaments. It keeps the ball portion of the shoulder, the humeral head, contained within the socket or glenoid. The capsule provides this stability, but still allows the shoulder to have a big range of motion.
Causes
The reason behind the development of adhesive capsulitits or frozen shoulder is largely unknown. I medical terms this is often called “idiopathic.” The most popular theory holds that adhesive capsulitis of the shoulder is an autoimmune reaction whereby the body’s immune system attacks itself. For example, one might catch a virus. A protein molecule on the virus may be similar to a protein molecule present on the capsule of the shoulder joint. The stimulated immune system then attacks the capsule causing an imflammatory reaction. When the capsule gets inflammed, it becomes painful and contracted causing the shoulder to lose motion.
We also know that trauma or surgery to the shoulder for other reasons can start the process. Unfortunately, it is impossible to predict at this time who might be predisposed to developing adhesive capsulitis. Breast cancer patients, ICU patients, and heart patients are at increased risk. Frozen shoulder in diabetics tends to get stiffer and more difficult to treat.
Symptoms
The symptoms of adhesive capsulitis typically are pain and decreased range of motion. There tends to be more pain at the extremes of motion. Other types of shoulder problems can lead to similar symptoms, so it is important to get a proper diagnosis.
Diagnosis
The diagnosis is usually made clinically. That is, by examining the patient and hearing the history of their symptoms. There is a typical natural history that patients go through.
There is an early “active stage” during which the pain and stiffness are getting worse. Following this is a ” frozen stage” where the pain often improves, but the shoulder might still not move so well. Finally, there is a ” thawing stage” during which the pain goes away and the motion returns. It can take several months even up to a year and a half to go through the typical natural history.
MRI scans and plain shoulder x-rays are usually normal, but are sometimes helpful in ruling out rotator cuff tears and glenohumeral joint arthritis that can give similar symptoms.
Treatment
The good news about adhesive capsulitis is that it typically gets better by itself. Again, it will go through the 3 stages described above, and it can take several months to get full return of painless function.
Initial treatment now that the proper diagnosis is made should be directed at 1) maintaining a functional range of motion ( keeping it from getting worse), and 2) decreasing the inflammation. Aggressive anti – inflammatory medicine initially is key to treatment. Physical therapy is important mainly to teach you the range of motion exercises that then should be done a little bit every day. Cortisone shots don’t play a big role here, but can be used as a fluoroscopic – guided intra – articular injection for refractory cases.
Unresolving cases in the thawing stage can be treated with a manipulation under anesthesia ( MUA). This done too early doesn’t change the typical natural history, and range of motion of the shoulder can scar back down.